Obsessive-Compulsive Disorder (OCD)
- Armaan R
- Aug 4
- 4 min read
Part One: What Is It?

Introduction
Obsessive-compulsive disorder (OCD) is a mental health presentation that can be highly debilitating and interfere with one’s professional, personal, and recreational endeavours. Despite the substantial impact of OCD, I find that many of my prospective clients, and the general populace, may not be aware of its intricacies. Therefore, I would like to provide some awareness regarding this disorder, and how it can be treated through a combination of medication and psychotherapy.
Symptoms
According to the Diagnostic and Statistical Manual of Mental Disorders:5th Edition – Text Revision (APA, 2022), the diagnostic markers for OCD include:
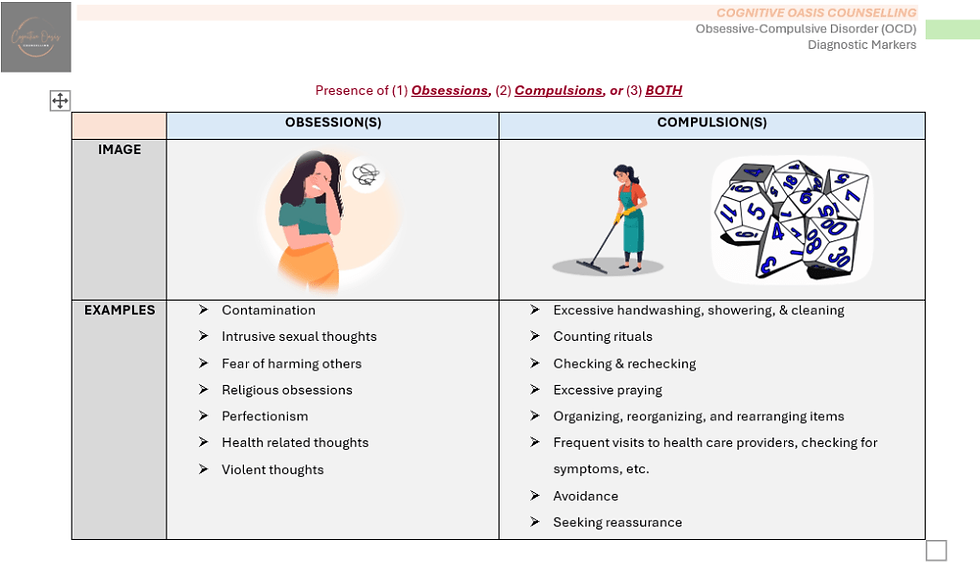
The presence of (1) obsessions, (2) compulsions, or (3) BOTH.
Obsessions are defined as:
Intrusive and unwanted thoughts, urges, and/or images that cause substantial anxiety and distress.
Compulsions are defined as:
Repeated behaviours or mental acts that an individual is driven to perform to minimize anxiety and distress caused by obsessions.
The obsessions and compulsions are time consuming (>1 hr. per day), and cause impairment in various facets of one’s life.
The symptoms of this condition cannot be explained via the use of a substance (drug, medication, etc.) or an alternative medical ailment.
Furthermore, individuals with OCD can present with varying degrees of insight (APA, 2022):
Fair Insight.
Individuals acknowledge that their obsessions are definitely, or probably, not true.
E.g. A client is aware that he will definitely, or probably, not get sick if he doesn’t wash his hands six times.
Poor Insight.
Individuals believe that their obsessions are probably true.
E.g. A client believes that he will probably get sick if he doesn’t wash his hands six times.
Absent Insight (Delusional Beliefs).
Individuals believe that their obsessions are completely true.
E.g. A client believes that he will definitely get sick if he doesn’t wash his hands six times.
Based on clinical experience, I find that individuals, with OCD, present with obsessions and compulsions, as compulsive behaviour is instrumental in minimizing, or mitigating, the anxiety, distress, and worry generated by their obsessions. Furthermore, most of my clients have fair insight regarding the validity of their obsessions. For this reason, they often express that they are “going crazy,” as their obsessions persist despite trying to rationalize their thoughts (also a mental compulsion).
Prevalence
From a statistical perspective, a small number of individuals are formally diagnosed with OCD. A study conducted by Osland et al. (2018) found that a mere 0.93% of Canadians received an OCD diagnosis. In the United States, approximately 1 in 40 adults will develop, or have, this condition during their lifetime (Ruscio et al., 2010, as cited in IOCDF, 2025). Additionally, 1 in 100 kids, and teens, have OCD in the United States (Browne et al., 2015, as cited in IOCDF, 2025; Geller et al., 2021, as cited in IOCDF, 2025).
Within my clinical practice, I see many clients whose symptoms are a strong indicator for OCD; however, they have not received a formal diagnosis or are unaware of this condition. When appropriate, I impel them to speak to their primary care physician, regarding a referral to a psychiatrist, or psychologist, for an assessment and diagnosis.
Comorbid Conditions
Individuals with OCD often present with one, or more, simultaneous medical conditions. These include (1) lifetime anxiety disorders – 76%, (2) depressive and/or bipolar disorder – 63%, and (3) substance use disorder (SUD) – 39% (APA, 2022). Furthermore, nearly 22% of individuals with OCD have a simple phobia during their lifetime (Tsao et al., 2024).
I have seen many clients with OCD that also engage in mild-moderate substance use on a consistent basis. This includes, but is not limited to, alcohol, marijuana, and nicotine consumption. Mancebo et al. (2009) conducted a study, with a sample size of 323 participants with OCD, and found that 27% of these individuals met lifetime indicators for a SUD. Many of my clients convey that they engage in substance use as a way to self-medicate and reduce anxiety and distress caused by their obsessive thoughts.
Treatment
Treatment for OCD entails a combination of medication and psychotherapy utilizing an approach called Exposure and Response Prevention (ERP). ERP is a type of Cognitive Behavioural Therapy (CBT), and is very efficacious in treating OCD.
I will provide insight into ERP, in a subsequent post, shortly. More to come.
References (Sources)
American Psychiatric Association (APA). (2022). Obsessive-compulsive and related disorders. In Diagnostic and statistical manual of mental disorders (5th ed., text rev.).
Mancebo, M. C., Grant, J. E., Pinto, A., Eisen, J. L., & Rasmussen, S. A. (2009). Substance use disorders in an obsessive compulsive disorder clinical sample. Journal of anxiety disorders, 23(4), 429–435. https://doi.org/10.1016/j.janxdis.2008.08.008
Osland, S., Arnold, P. D., & Pringsheim, T. (2018). The prevalence of diagnosed obsessive compulsive disorder and associated comorbidities: A population-based Canadian study. Psychiatry research, 268, 137–142. https://doi.org/10.1016/j.psychres.2018.07.018
Tsao, S., Yusko, D., DiChiara, C., Murphy, S. (2024, January 24-26). Obsessive compulsive disorder: Diagnosis, assessment, and treatment with exposure and response prevention. Center for Anxiety Behaviour Therapy. https://www.centerabt.com/
Who gets OCD? (2025). International OCD Foundation (IOCDF). Retrieved July 28, 2025, from https://iocdf.org/about-ocd/who-gets-ocd/#note-63-4



Comments